We have entered an era of exceptional confluence between different disciplines, technologies, and institutions that contribute to emerging techniques in neurosurgery. From stem cells to nanotechnology to genomics and drug delivery, this will truly be the neuro-centric age, which is rather timely since, we are also entering an era where neurological disorders, from dementia to spinal pain are reaching epidemic proportions. Today I will concentrate on two of the areas where innovation has provided better solutions for performing surgery.
[To read more of Amir Vokshoor’ s thought leadership click here]
Better Implants
Cervical spine disc problems can occur from overuse, after an accident or just wear and tear. The damaged disc can either cause direct pain in the spine or referred pain by pinching the adjacent nerves which can cause excruciating pain in the neck and arms. In severe cases a disc herniation can cause severe pressure on the spinal cord and lead to paralysis. I am always searching for new ways of improving my patients’ outcome from spinal surgery with faster recovery and return to activities. Placing an artificial disc instead of performing a traditional fusion allows us to replace the damaged disc without sacrificing natural motion, paramount to long-term recovery and an active lifestyle. Before artificial discs were available, patients would undergo a fusion procedure where a bone graft or spacer is placed to restore the height of the disc and relieve the pinching of the nerves. This would result in loss of motion in that spinal segment. This in turn can cause additional stress on the adjacent spinal segments. An artificial disc like Mobi-C is an alternative to the fusion to restore the height and remove pressure on pinched nerves. The innovative design mimics natural spinal motion and allows my patients to recover from incapacitating neck and arm pain, and avoid the serious consequences of nerve damage, such as weakness or numbness. Additionally nerve healing may be enhanced by therapy, neuro-stimulation, and in the very near future, stem cell technology. I will expand on these topics in future issues.
Better Optics
Since the advent of micro-neurosurgery in the latter half of the 20th century, neurosurgical techniques in the spine and the brain have enjoyed a convergent path of ever evolving technology to improve the optics and ergonomics of the operating microscope. The Zeiss pantero microscope is a truly remarkable product of design and innovative technology allowing the surgery to be performed with much smaller incisions as well as minimizing trauma to the muscles and soft tissues during surgery. With the latest model of Zeiss Pantero, We have been able to perform micro-neurosurgery even more delicately with meticulous protection of nerves and the spinal cord. As an example, our better optics have revolutionized one of the traditional surgeries such as the direct lateral lumbar interbody fusion. The reported complications associated with this approach included local trauma to the psoas muscle as well as nerve damage from direct injury or stretch of the lumbar plexus. Our group has described a microscopic approach using the latest model of Zeiss Microscope to further minimize the surgical trauma to the psoas muscle and the lumbar plexus. We reviewed our experience with this novel technique, for the goal of minimizing the retraction trauma on the psoas muscle and for direct visualization and protection of the neural structures. We believe this technique adds critical safety to the laterally approached spine.
Age of Personalized Care
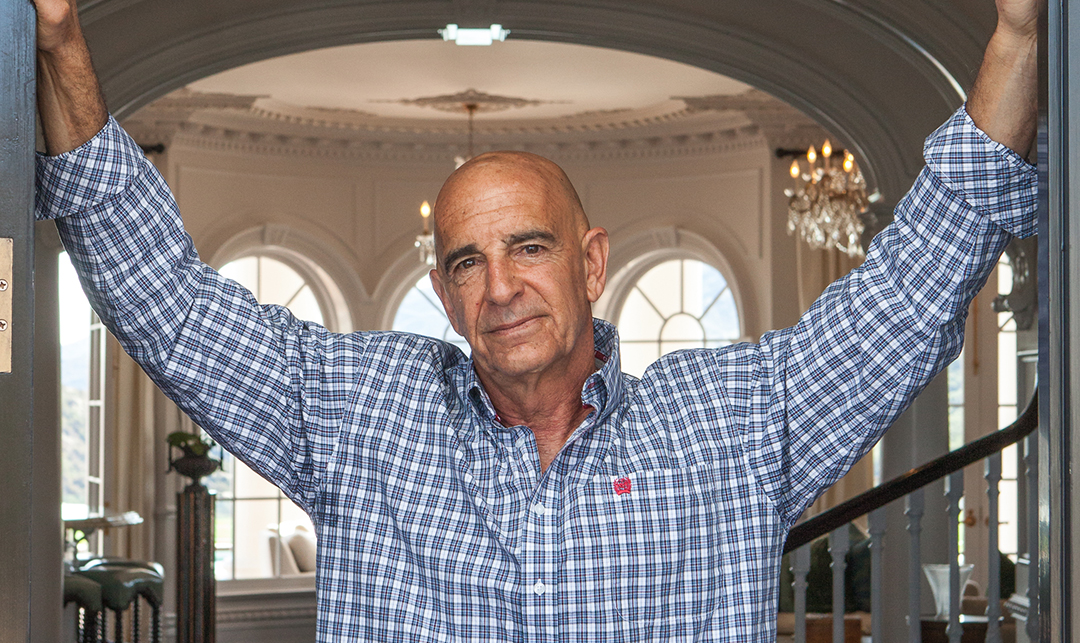
One of the scariest moments in anyone’s life is realizing that surgery is needed to improve function, get rid of pain, or prevent nerve damage. My most important job as a neurosurgeon is to provide a comprehensive plan of my patients return to wellness and to declare whether surgery is paramount for achieving this goal. Clear, honest, scientific review of the success rates of each surgical strategy needs to be considered, to provide clarity through the fog of multitude of information sources. Most of the time surgery is an absolute last resort, but sometimes it is truly the only way to restore one’s function, and prevent further nerve damage. The goal of surgery should always be considered as a part to the whole path of return to wellness. We are collaborating with large national data registries to provide our patients with the most up to date research on success rates from various strategies. In the information age, sifting through the data will be as important as performing life-saving surgeries. With our method, the patients assume the CEO role for their health and get informed by their doctor in the most personal setting to make the right decision for their health.
[For more on the Institute of Neuro Innovation’s approach click here]
From the realm of imagination to live action, these technologies have truly advanced my ability to help my patients. I believe artificial disc technology will continue to advance, as more minimalistic interventions are designed for addressing pain, restoring function, and enhancing lives.